Learning to infuse is an important part of your long-term health care and it takes some time to learn. At this stage you probably have learned or are starting to learn to self-infuse. Your health care provider or HTC team will help you learn how to infuse. This guide will walk you through it step by step. You will be on the way to infusing before you know it!
This section of Infusions Basics covers:
Setting the Stage for Safe Infusion
Information About Getting Into a Vein
Setting the Stage for Safe Infusion
You will practice the steps for safe infusion together with the HTC team or health care provider before you infuse by yourself. You can also contact your HTC team with questions as they come up. There are different ways to access a vein and your HTC team will work with you to determine the best way to do this.
It is important to be organized and to have a clean workspace that is free of clutter. Gather all the supplies and medications needed to do your infusion. There are general safety guidelines that everyone who infuses should follow to prevent infection:
- Clean your space before you begin the infusion. Clean means your workspace is free of dirt. Sterile means germ free, and you will need to use cleaning supplies like bleach or isopropyl alcohol to clean your work area.
- Wash your hands and arms up to the elbow with soap and warm water.
- If doing an infusion on someone else, it is good to wear gloves during the infusion and while throwing away the used supplies.
- Put used needles and bloody gauze in your sharps container.
- If you spill blood in the workspace, use chlorine bleach to clean it.
Tips to Keep Supplies Sterile
Some of the supplies you will use to do the infusion are sterile and you will need to take care that they are kept sterile during the infusion.
Here are some tips to keep supplies sterile:
- The infusion needle will come in a sterile package, and it must be kept sterile after you open it.
- If the needle touches anything (even a table that has been cleaned), the needle is no longer sterile and needs to be thrown away.
- Always use sterile alcohol pads.
- Never reuse or share needles.
Information About Getting Into a Vein
There are different ways to access or get into a vein. Your HTC team will work with you to determine the best way to do this. Two ways are putting a needle directly into the vein or using a special device called a port that will help make the process a bit easier.
Using a Port (Central Venous Access Device) (CVAD)
When infusing into a vein is too difficult, some patients may decide to use a central venous access device (CVAD) also called a port. A port is a device that is surgically inserted under the skin and connected directly to a vein. This allows a person to inject the medication into the port rather than having to inject directly into the vein. It is used more often in children, but adults can also find it useful. There is more of a risk for infection using a port as compared to using a vein1,2. Talk to your health care provider to figure out what will work best for you.
Tips to Prepare Your for an Infusion
Finding your vein for infusion can be hard. These suggestions will help you feel ready and confident to find a vein, whether it is your first time infusing or you’ve been infusing for years.
- Make sure you have had plenty of water to drink before you begin. This will help the veins to be seen easier.
- Do a little exercise first like going for a walk or some other way to move your body. This will help to raise your blood pressure so the veins can be seen easier.
- A warm bath or shower may be relaxing and will help you to find a vein. Apply a warm washcloth to the desired infusion site (Remember to clean the area again before you infuse).
Steps To Do an Infusion
1. Gather supplies.
2. Make sure the workspace is well lit.
3. Clean your work area before you begin using a sterile alcohol pad. If you would like, you can also place down a clean cloth or disposable pad to work on.
4. Wash your hands and arms up to the elbow with soap and warm water.
5. Put on gloves (wearing gloves is required if you have a port or for anyone helping with your treatment).
6. Mix factor and pull the medication into the syringe which is explained in the guidelines that come with your medication (the package insert). You can also find information on how quickly you will need to finish the infusion before the medication is no longer good to use.
1. Find a comfortable position with your arm resting on a firm surface.
2. Use a tourniquet to help you decide the best vein to use.
a. Using a tourniquet will allow the vein to become full and larger feeling. Place the tourniquet 3 to 6 inches above where you would like to do the infusion.
b. If looking at veins in the arms, ask your to make a fist or dangle their arm which will allow the veins to become bigger.
3. Use your finger to feel for and trace the direction of the vein.
4. Gently slap the skin at the infusion area. This can help visualizing the vein.
5. Finding a vein can be tricky. Follow the tips above.
1. Clean the site by using a sterile alcohol pad and rubbing in a circular motion from inside to outside the area.
2. Allow the skin to dry. Do not touch the clean site before you insert the needle.
1. With the angled surface (known as the bevel) of the needle up insert the needle into the vein at an approximately 30-degree angle. This means not directly straight down on top of the vein and not flat into the vein but somewhere in between.
2. Once the needle has entered the skin you can adjust the needle to go a little deeper into the vein.
3. Pull back on the syringe slightly to check for a blood return. A blood return is when you pull back on the syringe slightly and blood enters the tubing connecting the needle to the syringe. A blood return lets you know you are in the vein. Sometimes you might get a blood return without pulling back on the syringe.
4. Open the tourniquet.
5. Gently push the factor into the vein while watching the area where you inserted the needle for any issues, like factor leaking out of the vein. Some things to watch for are swelling, redness, and pain at the infusion site. If you think you are having this problem, stop infusing and remove the needle.
6. If you need to begin again to finish infusing the factor, you will need to attach a new needle to the syringe and start by cleaning the site again.
7. Once all the factor is infused remove the needle and put it in the sharps container.
1. Apply pressure to the infusion site using a gauze pad once completed and keep pressure for a minimum of 5 minutes. Then apply a bandage.
2. If you spilled factor or if there is blood on your work area, use chlorine bleach to clean it.
3. Log your infusion in your treatment log.
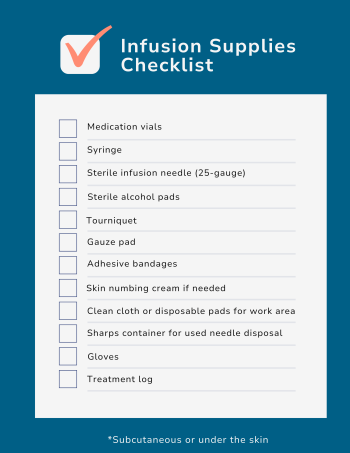
Here is a checklist to easily follow the step-by-step process:
Treatment Logs
Your treatment log should be kept in a safe place that you can get to easily, and you should bring it to all your medical appointments. It’s also a good idea to let a loved one know where they can find your treatment log in the event of an emergency. The best treatment log is one that you will use. So, find the best one for you.
A treatment log is a record of all your infusions and any bleeds you might have. Here are some of the reasons why keeping a well-organized treatment log might come in handy:
The treatment log gives information to your HTC or other health care providers about how well your medication and treatment plan are working. After reviewing their treatment log, your healthcare provider may decide to change your medication dose, change your treatment plan, and identify target joints.
Insurance companies also use information from your treatment log to watch how bleeding symptoms are managed, review the effectiveness of treatment, and for insurance reimbursement. Not all insurers require treatment logs, but some do.
A treatment log can be helpful if you are applying for disability or financial help from the U.S. Social Security Administration on behalf of your. With documentation of bleeding episodes and factor infusions or other treatments, this information log helps describe how your daily activities are affected by the bleeding disorder. The treatment log can be very useful in a disability application.
Sometimes a manufacturer may recall medication due to patient safety concerns. Keep a record of the name, lot number, and manufacturer of your medications so that you can figure out if your could be affected by the recall.
The treatment log gives your health care provider and HTC a record of how you have managed your bleeding disorder. A treatment log should track all factor infusions, treatment information, and all bleeds. As your becomes older, they can record the information in their logs.
Each time you or your infuse, you should record:
- The date and time of the treatment
- Information on the medication used (include the brand name, the expiration date, the lot number, and how much was given)
- The reason for the treatment (for example: scheduled prophylaxis, pre-surgery, injury)
If your has a bleed, you should also record:
- The date and time of the bleed
- Where the bleed is in your body and information about the bleed (how long it lasted, level of pain)
- What was the cause of the bleed (for example: fall, blowing nose, unknown)
- The treatment plan for the bleed from your HTC or health care provider
- Additional steps taken to manage the bleed (for example: pain medication, ice pack, bandages with pressure)
The treatment log gives your healthcare provider and HTC a record of how you have managed your bleeding disorder. A treatment log can be kept by writing down information in a notebook, a file on your computer, or you can keep an electronic log using a mobile app. Some apps allow you to share your records with your healthcare provider or HTC. There are many treatment log apps. Keep in mind how the app will use your information.
Needle Fear and Phobia
Needle fear and phobia is a common issue. Here is a video that will give you information and tips to tackle needle fear and phobia:
1. Santagostino, E., & Mancuso, M. E. (2008). Barriers to primary prophylaxis in hemophiliac children: the issue of the venous access. Blood transfusion = Trasfusione del sangue, 6 Suppl 2(Suppl 2), s12–s16. https://doi.org/10.2450/2008.0031-08
2. Titapiwatanakun R, Moir C, Pruthi RK, Stavlo PL, Schmidt KA, Rodriguez V. Central venous access devices for paediatric patients with haemophilia: a single-institution experience. Haemophilia. 2009 Jan;15(1):168-74. doi: 10.1111/j.1365-2516.2008.01906.x. PMID: 19149849